Informatics ApproachesInnovationPartnershipTherapeutic “Trust me, I’m an AI doctor” – using Artificial Intelligence to prevent sepsis-related deaths

Imperial researchers have developed an Artificial Intelligence system that could be used to personalise the treatment of patients with sepsis in real time. The computational model, known as ‘AI Clinician’, learned the best individual treatment strategy from medical records of almost 100,000 sepsis patients, and provided recommendations that proved more reliable than decisions made by human doctors.
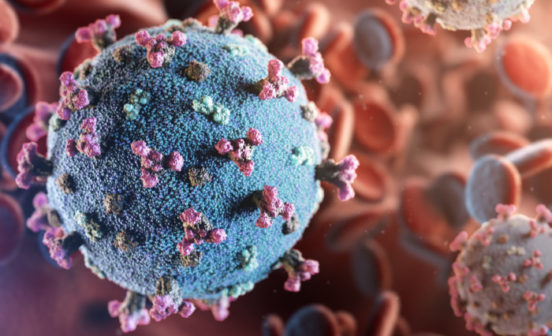
Sepsis, or blood poisoning, is a severe complication of an infection that leads to life-threatening acute organ dysfunction, and kills ~44,000 every year in the UK. The condition is managed by giving intravenous fluids and in severe cases, vasopressors- a medication that causes tightening of blood vessels, thereby increasing blood pressure and maintaining blood flow. However there are no clear indicators of when vasopressors should be started, or how much fluid should be given, leading to extreme variability and sub-optimal treatment, resulting in poor patient outcomes.
To help doctors maximise a patient’s chance of survival, Imperial researchers ‘trained’ an AI system to analyse individual patient’s vital signs and recommend the best treatment strategy. The results, published in Nature Medicine, revealed that 98% of the time, the AI system matched, or was better than, the treatment decision made by a human doctor, with lowest mortality in patients where the human doctor’s doses of fluids and vasopressor matched the AI system’s suggestion. On the contrary, when the doctor’s decision differed from the AI system, a patient had a reduced chance of survival.
NIHR Research Professor Anthony Gordon, an Imperial BRC researcher and senior author of the study, explained further: “The AI Clinician was able to ‘learn’ from far more patients than any doctor could see in a lifetime. It has learnt from 100,000 patients and ‘remembered’ them all equally whereas doctors are always susceptible to recall bias, where they particularly remember recent cases or unusual cases”.
Dr Also Faisal, senior author from the Department of Bioengineering and the Department of Computing at Imperial, added: “An intensive care doctor will see roughly 15,000 patients by the time they retire. Yet this system has seen nearly 100,000 patients, it has the life time experience of 8 doctors, and has learned from each of those cases what the best decisions were for each situation.”
The next step for AI Clinician is to trial it in UK hospitals, and prospectively assess decision making using real-time data. This cutting-edge work is a direct result of the unique Imperial BRC ethos that brings together engineers and clinicians to solve real health problems and improve healthcare. It was led by Dr Matthieu Komorowski, a clinician who obtained a PhD in Artificial Intelligence with the two senior authors. Dr Faisal commented: “We broke down boundaries and silos that held back traditional approaches to healthcare, by training a novel generation of PhD students to look at AI and Healthcare as one problem, not two.”
The work was supported by the Engineering and Physical Sciences Research Council (EPSRC) and NIHR Imperial BRC. You can read the original press release, including a statement from Health Minister Lord O’Shaughnessy, here.