Therapeutic Clinical translation of endothelial colony forming cells

Endothelial cells line the interior surface of blood vessels, and serve a number of important purposes to maintain the organism functioning properly. Firstly, endothelial cells provide a selective barrier between the blood and tissues, across which nutrients and cells can move. Secondly, endothelial cells controls crucial processes such as inflammation, haemostasis (i.e. the formation of clots) to stop bleeding, and vascular tone to respond to changes in blood pressure or requirement of oxygen. Thirdly, endothelial cells drive the formation of new blood vessels, a process called angiogenesis, which is essential for tissue repair, wound healing and the menstrual cycle, and is also essential for regenerative medicine strategies.
Endothelial dysfunction is a crucial event which precedes the development of atherosclerosis, a chronic disease that is the result of a build-up of fatty plaques in the walls of arteries. Well-established risk factors for atherosclerosis are high blood pressure, diabetes, high cholesterol and smoking, which all chronically activate the endothelium. Measurement of endothelial dysfunction, as the inability of the arteries to dilate fully, has been shown to be a significant risk factor for stroke and heart attacks. More detailed and molecular analysis of endothelial cell function would be valuable for many diseases, but access to these cells has always been a challenge.
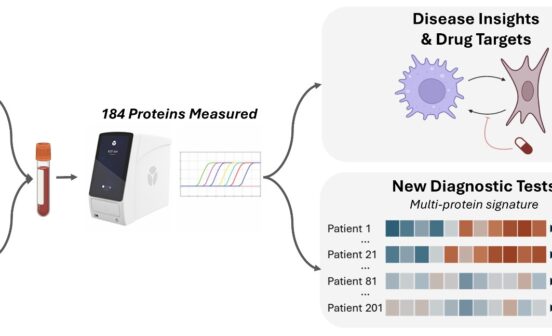
A breakthrough in this area came when circulating endothelial progenitors (called endothelial colony forming cells or ECFC) were discovered about 20 years ago; these provide access to endothelial cells from patients in a non-invasive way, from a simple blood sample. ECFC cells can be used as liquid biopsies to study multiple aspects of endothelial dysfunction, provide new information on mechanisms of disease and could be used as a tool to stratify (arrange or classify) patients depending on their risk, to help clinical decisions Studies on ECFC can also reveal new candidate therapeutic targets.

Imperial researchers have been using ECFC to study cardiovascular, respiratory and haematological diseases for many years. Here, they reviewed scientific publications which have used ECFC to investigate endothelial abnormalities in several diseases, including blood (haematological) disorders, pulmonary arterial hypertension, ischemic heart disease, chronic lung disease, diabetes and pregnancy-related disease, to understand how these findings can deliver translational patient benefit. In addition, investigators are using ECFC for gene therapy and tissue bioengineering. For example, ECFC have been investigated for engineered bioartificial vascular structures and have shown to be able to support the development of vascular networks and tissue regeneration. Other studies have identified new mechanisms of disease and opened the potential for a new way of treating patients.
Dr Koralia Paschalaki (lead author and post-doctoral Clinical Research Fellow), supported by the NIHR Imperial BRC Cardiovascular Theme, said: “ECFC isolated from blood samples have been proven an invaluable resource for molecular studies on blood vessels’ dysfunction in several diseases. Current studies investigate how we can use these cells for gene therapy, personalised and regenerative medicine with very promising results.”
Professor Anna Randi, Professor of Cardiovascular Medicine at the National Heart and Lung Institute and Principal Investigator in the NIHR Imperial BRC Cardiovascular Theme, said: “Since circulating endothelial progenitor cells were first identified, they have transformed our ability to study diseases that involve blood vessels. At Imperial we have focused on cardiovascular, respiratory and haematological disorders, but this review demonstrates that studying ECFC can potentially be beneficial to many other disease areas.”
The researchers state that future studies aim to address current obstacles and help develop the use ECFC in clinical settings for regenerative approaches.