DiagnosticInformatics ApproachesPreventionTherapeutic Clinical description and outcome of hospitalised COVID-19 patients
Clinical characteristics and outcomes for hospitalised COVID-19 patients in the UK are important to guide the national response to this pandemic and emerging evidence suggests ethnic minorities might be disproportionately affected.
Imperial researchers undertook a retrospective cohort study to characterise the main risk factors associated with in-hospital deaths on patients hospitalised with laboratory-confirmed SARS-CoV-2 infection across hospitals from Imperial College Healthcare NHS Trust between February 25th and April 5th 2020, and evaluated whether the outcomes for these patients vary by ethnicity.
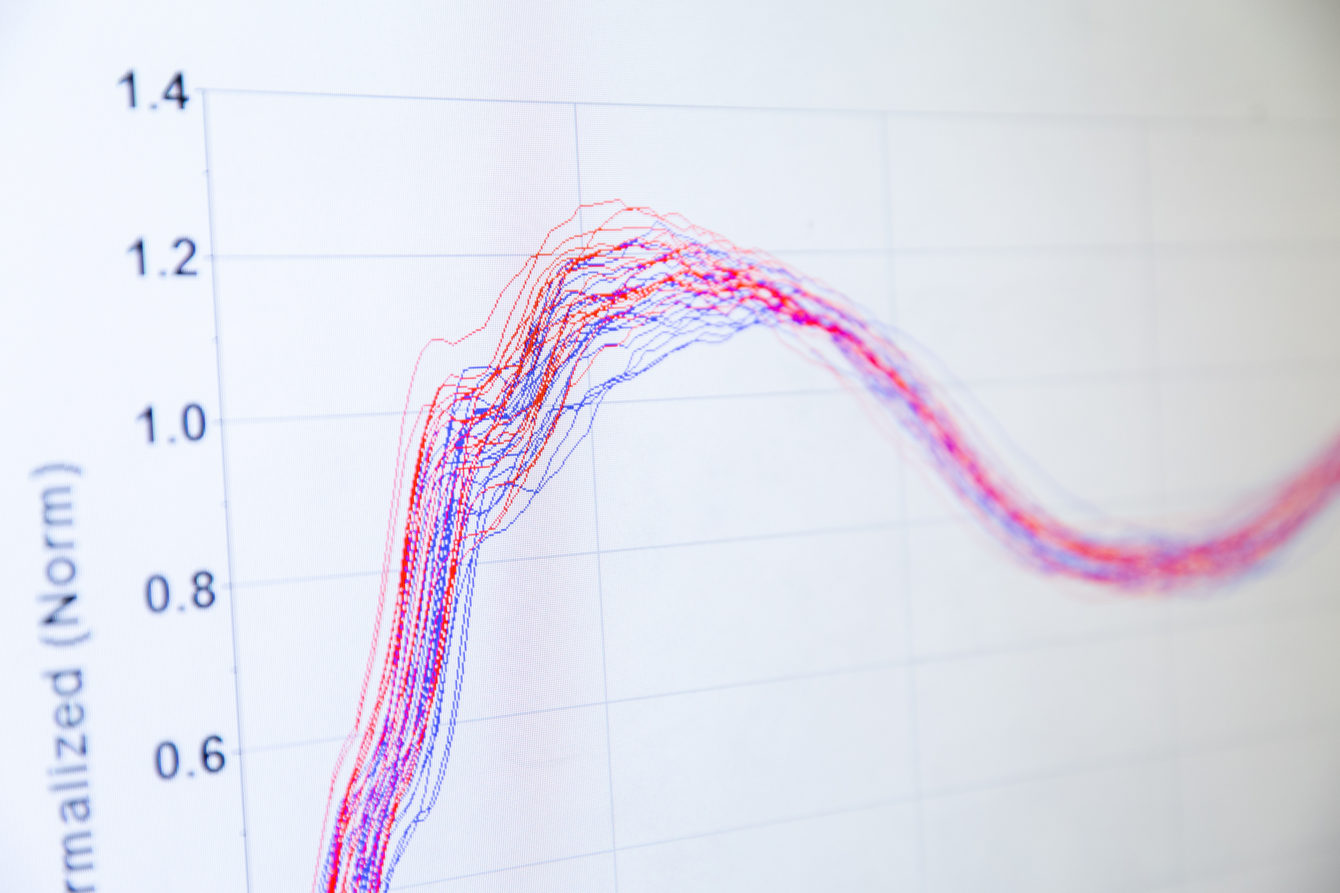
The report describes results from 520 patients, of which 302 (68%) had been discharged alive, 144 (32%) died and 74 (14%) were still hospitalised at the time of analysis. Several factors including increased age, male sex, high number of co-morbidities, reduced oxygen levels (hypoxia) on admission and certain admission blood tests (low blood platelet count, renal failure, low albumin and raised bilirubin levels) were associated with increased mortality in hospital.
The study found that a larger proportion of patients admitted to hospital were from ethnic minority groups when compared with last year’s admissions at Imperial College Healthcare NHS Trust: 40% of patients were from black and Asian minority groups, 38% white and 22% ethnicity was unknown. There was no overall difference in mortality between different ethnicities. However, patients of black ethnic minority were younger and had fewer pre-existing health conditions compared with those of white background. With these factors taken into account, an emerging trend suggests that patients with black ethnicity may be at increased likelihood of mortality. The researchers recommend that research is urgently expanded to see whether this pattern is replicated on a national level to better understand whether socio-demographic and biological factors could be driving differences in the COVID-19 epidemic at the community level.
Dr Shevanthi Nayagam, senior author of the report and part of the NIHR Imperial BRC Gut Health and Infection & AMR Themes, said: “We found that patients from BAME groups were over-represented in admissions for COVID-19 compared to a normal year with other illnesses. Once in hospital, patients with a black ethnic background, were younger and even though they had fewer pre-existing conditions, they tended to show a similar severity of illness than older patients from white ethnicity. It is critical that we understand whether this pattern is true across the UK and what the potential key drivers of these differences are.”
The study used routinely collected non-identifiable clinical audit data approved by the Imperial College Healthcare NHS Trust clinical governance team.
This is the 17th report on the COVID-19 outbreak released by the WHO Collaborating Centre for Infectious Disease Modelling within the MRC Centre for Global Infectious Disease Analysis, J-IDEA, Imperial College London. This report is a collaboration with the Division of Digestive Diseases, Department of Metabolism Digestion and Reproduction, Department of Infectious Disease, Department of Primary Care and Public Health, School of Public Health, NIHR Imperial BRC and Imperial College Healthcare NHS Trust.