DeviceDiagnosticPrevention MRI scan is a superior screening test for prostate cancer
Results from the first clinical trial demonstrated that a 15-minute scan was better at detective aggressive prostate cancer than conventional PSA blood test.
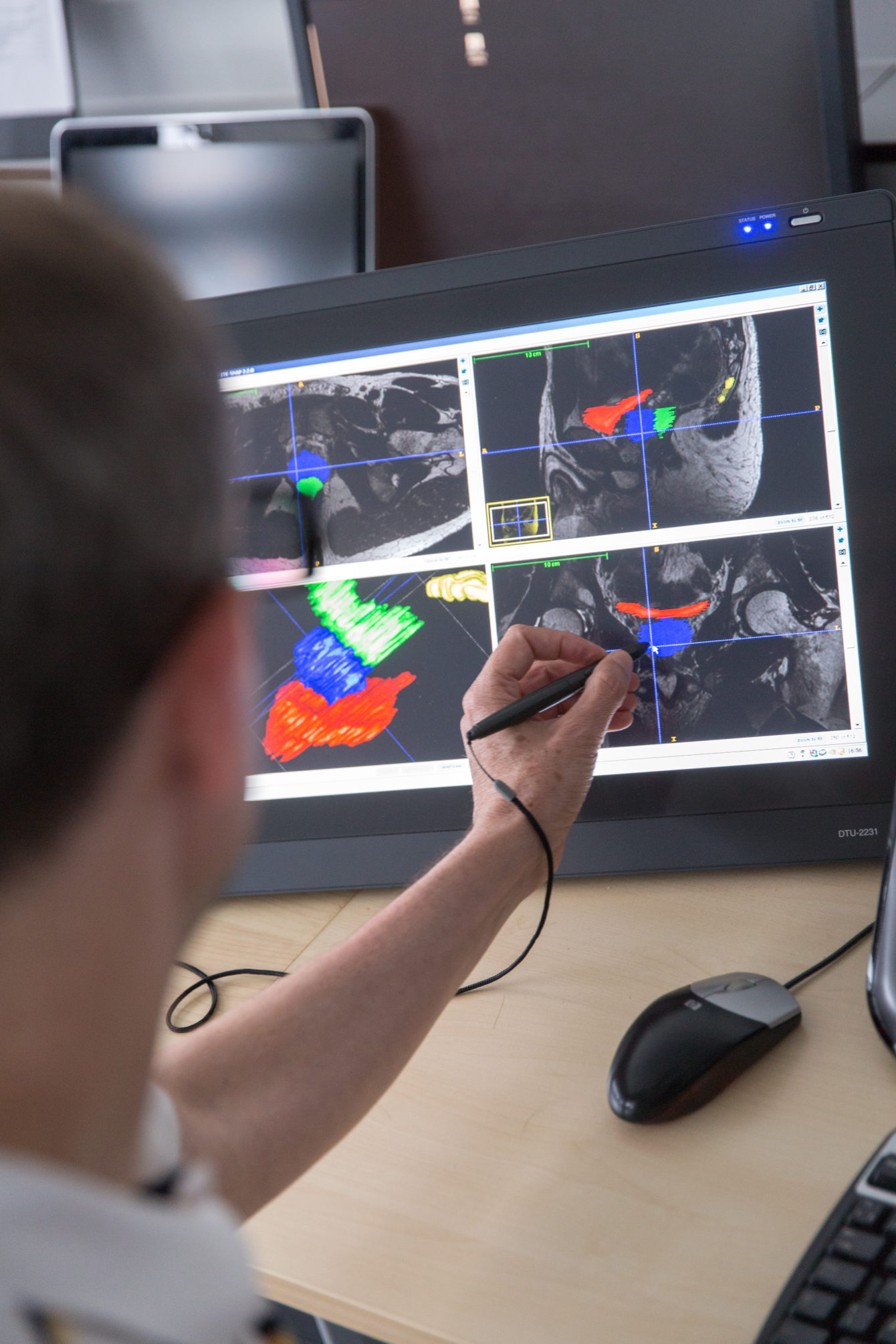
PROSTAGRAM (PROstate Cancer Screening Trial using A Group of Radiological Approaches including MRI and ultrasound) trial tested the performance of a short MRI and ultrasound as screening tests for detecting clinically significant prostate cancer. It aimed to address an unmet need for alternative screening tests to PSA (prostate-specific antigen) blood test, which has several limitations.
Professor Hashim Ahmed, the senior author and a researcher from the Surgery and Cancer BRC Themes, told the news that the development has been hailed as a “game changer”.
“The number of aggressive prostate cancers missed by PSA highlights the importance of ramping up our research efforts into alternative ways to screen for prostate cancer. MRI has the advantage of passing over the many cancers which don’t need to be diagnosed and focusing on the types of cancers which are more likely to shorten life.”
“By finding these aggressive cancers at the earliest opportunity, men have the opportunity to be offered less invasive treatments with fewer side effects.”
PROSTAGRAM recruited 411 volunteers aged between 50 and 69 years of age in record time (recruitment was completed 19 months ahead of schedule). Volunteers were screened using both, PSA and a 15-minute MRI tests. The new 15-minute MRI scan is a shorter version of the 40 minute MRI scans that are used for men referred to specialists by their family doctor.
Results of the study, presented at ASCO 2020, demonstrated the short MRI with a screen-positive threshold of score ≥ 4 had a similar biopsy rate compared to PSA (~10%) and detected the majority of significant cancers. It was well-tolerated as a screening test, as only 2 men were unable to complete the short MRI protocol. Importantly, the PSA test missed 10 significant cancers with a sensitivity and specificity of 41.2% and 63.6% respectively.
Taken altogether, this non-invasive test is not only more accurate at predicting prostate cancer and reduce over-diagnosis, it may also encourage more men to have a prostate check. Dr David Eldred-Evans, Imperial BRC researcher working on this study, said: “Unfortunately men can often be put off from seeking medical advice for prostate issues because they are worried about the need for a rectal examination,” and he hoped that results of this study “may encourage more men to have a prostate health check”.
This trial was funded Wellcome Trust, with Clinical Trials Unit and Imaging support from NIHR Imperial BRC.





