Prevention Serious food allergic patients are frequently not being prescribed potentially lifesaving medication

New data presented by paediatric allergy consultant, Dr Paul Turner and colleagues at Imperial College London, show that many patients who have had a previous serious allergic reaction to food (anaphylaxis) are not being prescribed adrenaline autoinjector pens (AAI) that are used to treat these life-threatening reactions.
Both UK and International guidelines recommend that food-allergic people with a history of food-anaphylaxis should be prescribed AAI (for example, Epipen® or Jext®) together with an allergy action plan, so they (and their carers) can respond quickly if they have further anaphylaxis reaction.
The data, presented at the British Society of Allergy and Clinical Immunology UK conference, came from an analysis of over 130,000 UK patient records where food allergy was referenced between 2008 and 2018. Of these, 3,589 (2.7 per cent) mentioned an unplanned hospital encounter for anaphylaxis during this time.
Researchers found that 40 per cent of these patients with a previous anaphylaxis to food were not prescribed an AAI and 59 per cent were not given a repeat prescription, meaning they were left at future risk with devices going out of date.
Anaphylaxis is a serious and potentially life-threatening allergic reaction, which can be fatal. It can cause swelling of the airways, breathing difficulties and low blood pressure, and is considered a medical emergency. AAIs contain adrenaline, which is the best treatment for anaphylaxis. AAIs are designed to be used by patients themselves (or their carers) to improve symptoms of anaphylaxis before emergency medical services can help.
Researchers also found that children were 63 per cent more likely to be given repeat AAI prescriptions than adults.
Dr Turner, who is a clinician scientist in paediatric allergy and clinical immunology at Imperial College London, sees children and young adults with severe food allergies at St Mary’s Hospital. He is also leading several studies at Imperial College Healthcare NHS Trust and other hospitals in the UK, to help learn more about food allergy and find new ways to help patients at risk of anaphylaxis.
He said: “When you have a food allergy, it’s almost impossible to know if an accidental reaction might cause a severe reaction, so we always tell patients and their families how important it is to always carry your AAI with you.
“But this data shows that many patients who should absolutely be prescribed adrenaline are not getting this important medicine to use if they need to. We need to understand the reasons for this so that we can work with our colleagues in general practice and primary care to best provide for patients at risk of anaphylaxis.”
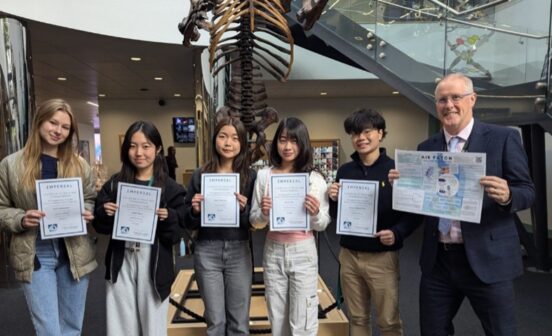
Dr Turner has also contributed to a new leaflet written by allergy experts and designed to give patients, families, friends and childcare providers more confidence about what to do in the event of an anaphylaxis reaction.
This research was funded by the UK Food Standards Agency. Clinical trials at Imperial College Healthcare are supported by funding from the National Institute for Health and Care Research (NIHR) Imperial Biomedical Research Centre (BRC), a translational research partnership between Imperial College Healthcare NHS Trust and Imperial College London, which was awarded £95m in 2022 to continue developing new experimental treatments and diagnostics for patients.
Reuben’s story
10-year-old Reuben is allergic to peanuts, tree nuts, sesame, fish and shellfish. He was also diagnosed with milk and egg allergy from four months old. He is cared for by Dr Turner and his team at St Mary’s Hospital.
Reuben’s first reaction was when he was just seven months old and tried salmon for the first time but he has had three more anaphylaxis reactions since then and is an expert in what to do if it happens again. Reuben always carries two AAIs with him that he can use himself and his parents, family members and school staff all also know exactly what to do in the event that he experiences an anaphylaxis reaction.
“The first signs that Reuben is having a serious reaction are that his throat begins to itch and then he starts wheezing, having breathing difficulties and becoming covered in a rash. That’s when we know we need to spring into action and use his Epi-pen.
“As the reaction develops, he also gets stomach pains and his ears, eyes and tongue swell. But anaphylaxis is unpredictable and each of his reactions has presented differently. His second reaction was uncontrollably crying. His third reaction, he was completely silent” said his mum, Karina.
Reuben has recovered well from his reactions but with serious allergies, avoiding exposure again in the future can be tricky – one of Reuben’s reactions was caused by sesame that had been baked into the dough of what appeared to be a plain bagel. Carrying two AAIs is vitally important for the family to be able to go about their normal daily life.
“I just wanted to wrap him up in cotton wool and never go out again, but I know that if we don’t start going back out and doing the things that we enjoy, it makes the fear grow more and then your world shrinks and then you’re not living your life.”
With support from Dr Turner, the family feel confident in managing Reuben’s allergies out and about, regularly eating out at restaurants and even looking forward to their first holiday abroad.