Prevention Harnessing Data to Transform Inpatient Diabetes Care
Utilising routinely collected data from the Imperial College Healthcare NHS Trust (ICHT), a PhD researcher, James Beveridge, is building a tool to help clinical staff locate and triage people in the hospital with diabetes in real time, enabling them to provide more timely care and prevent potential harm.
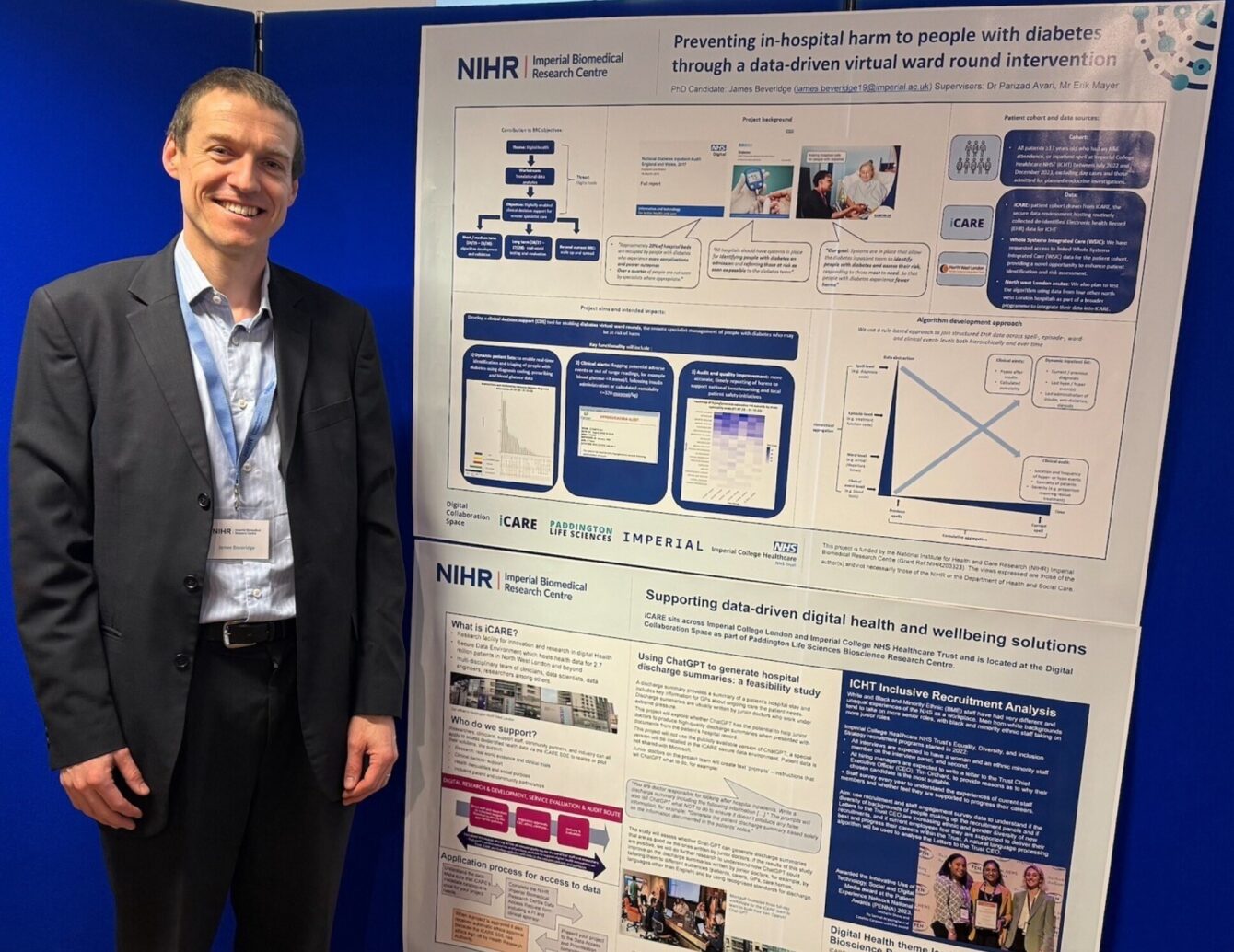
James Beveridge’s PhD project ‘Preventing in-hospital harm to people with diabetes through a data-driven virtual ward round’ is hosted by iCARE, a multi-disciplinary research team and secure data environment containing health data for Northwest London and beyond.
Project ambitions
Speaking to him about the project, Beveridge explained, “it is centred on the concept of ‘virtual ward rounds’, the remote specialist management of people in hospital who may be at risk of harm – one of the Imperial BRC Digital Health theme’s objectives. Instead of waiting for referrals, specialist teams like the diabetes team could more proactively identify people in hospital who need their input by using data already being collected in the hospitals electronic patient records (EPR). It’s a game changer, especially for conditions like diabetes, one of the most common chronic conditions in the UK, where people might often be in hospital for something else entirely, but their diabetes still needs careful management.
“We’re developing a clinical decision support tool that can pull relevant data in real-time – things like previous diagnosis information, recent blood sugar levels, what ward they’re on, how long they’ve been there, and more. The goal is to help the diabetes team spot people in hospital at risk of complications like persistent high blood sugars (hyperglycemia) or a low blood sugar event (hypoglycemia) and intervene earlier”, he said.
In developing the project, three core components have emerged. First, a Dynamic Patient List: A real-time list of people with diabetes in the hospital, showing their location, key clinical data, and indicators of risk. The diabetes team (who are not ward-based) could use the list to help prioritise which people in hospital to see first.
Then, Clinical Alerts: These are real-time pop-up alerts in the EPR that would be visible to all clinical staff, not just the diabetes team. For example, if someone has a hypoglycemic episode, an alert will guide the clinician on next steps. Currently, these kinds of alerts don’t exist.
Finally, a Clinical Audit Tool: This one’s retrospective – pulling data for national audits like the National Diabetes Inpatient Audit. Right now, staff must manually review records to find relevant cases. Automating this would save a huge amount of time and likely improve accuracy. We’re also looking at making the audit data interactive – so you can slice it by time of day or ward to spot trends and target quality improvements.
Next steps
However, Beveridge is only a year into the research project and a lot of time has been spent learning the skills necessary to execute it. He has been writing code that collates and links the relevant data from structured hospital databases and has also been working closely with the iCARE data engineers to enhance the dataset, adding new fields and improving the structure.
Beveridge explained, “I have built a prototype algorithm that identifies people in hospital with diabetes using a mix of diagnosis codes, blood tests, and prescribed medications. Diagnosis codes are tricky because they’re often only added after a patient is discharged, so we’re also using other indicators like medications to catch cases in real time”.
To help with the medical intricacies of proactively identifying people with diabetes diabetes, the project has a clinical sponsor, Dr Parizad Avari, a Consultant Diabetologist at ICHT and Clinical Lecturer at Imperial College London.
Dr Avari said that “by harnessing real-time data, we will transform diabetes care for people in hospitals, by taking a more proactive approach in preventing harm and enabling diabetes teams to work more efficiently.” She has been instrumental in providing clinical guidance, reviewing samples and refining the algorithm for initial validation work, according to Beveridge.
For Beveridge, “the next big step is linking hospital data with primary care records across North West London. Most diabetes care happens in primary care, and having access to that data would massively improve our ability to identify patients early, especially those who are new to the hospital trust and do not have any previous hospital records. It could also give us richer detail on other complications such as foot ulcers or eye disease, which are often not documented consistently in the hospital’s EPR ”.
Researcher profile
Beveridge started his PhD in November 2023. Before this, he did an MSc Health Policy at Imperial College London between 2019 and 2021, run by iCARE Director and Clinical Reader Dr Erik Mayer.
“I really got into research while working on my master’s dissertation, which looked at how hospital mergers affect the quality of care”, Beveridge said. “It was very quantitative using aggregated publicly available data. I really enjoyed it, but it also felt quite theoretical and it didn’t feel like it was making much of a real-world impact. That’s when I realised, I wanted to do research that’s more applied and directly related to patient care”.
Beveridge has also worked for NHS England for the past seven years. “I didn’t have a background in diabetes or working with hospital electronic patient record data”, he continued, “but this project sounded like exactly the kind of hands-on, real-world research I wanted to do.
“Honestly, I found that the more I put into this work, the more I get out of it. Learning to code, understanding data and working in interdisciplinary teams – it has all been really stimulating. It feels like I’m doing something that not only interests me but could also lead to real improvements in patient care. That’s a good place to be”, Beveridge said.
Presenting research
Recently, Beveridge presented a poster outlining his research project at the annual Imperial BRC event.
The event that took place on 25 March, brought together the 14 Imperial BRC themes and various associated projects for knowledge exchange and networking.
“Creating a poster helped me take a step back from the day-to-day coding and see the big picture”, Beveridge said. “It also helped me better understand how my project fits into the broader BRC objectives. I’m now starting to prepare for my early-stage PhD assessment, so having that opportunity to articulate the project clearly to an external audience was useful. Plus, it was nice to connect with other researchers and feel like part of something bigger”.
ICARE oversees the National Institute of Health and Care Research (NIHR) Imperial BRC Digital Health theme and provides access to health data in a secure data environment for research and innovation. iCARE also contributes to the OneLondon NHS England Sub-National Secure Data Environment programme.