We aim to understand what causes preterm birth (PTB), and how to predict and prevent it. For babies who are born preterm, we will study how to ensure that they are born in the best possible condition and the best ways to care for them in the neonatal unit and beyond.
Why this Research is Needed
Preterm birth is the leading global cause of death in children under five. Preterm survivors have dramatically increased risks of impaired neurodevelopment problems and chronic diseases and reduced lifespan. Mothers of preterm babies have increased risks of subsequent PTB, cardiovascular disease and diabetes. The UK PTB rate is 7.6%, higher than comparable-income countries. In our diverse North-West London community PTB is significantly higher in ethnic minorities, particularly black women. 30% of PTB occurs in the poorest communities and only 12% in those better off. Neonatal care is one of England’s costliest NHS services. Preventing PTB, improving mother-baby outcomes, developing diagnostics and therapeutics, and attracting industry investment are UK Government focuses.
Theme Aims
Use our large cohorts of mothers at risk of miscarriage and preterm birth, together with our expertise in studying bacterial host interactions and the immune system to understand the causes of spontaneous preterm labour, and to develop methods for diagnosis and treatment.
Study interventions to improve maternal cardiovascular function to reduce the risk of pre-eclampsia and fetal growth restriction.
Use our European network of fetal medicine centres to determine the best time to deliver a small baby.
Translate our development of High-Intensity Focused Ultrasound to improve outcomes in Twin-Twin Transfusion Syndrome.
Study cardiovascular stability and nutrition as key modifiable factors in improving neonatal outcomes and longer-term cardiometabolic health.
Harness the power of our National Neonatal Research Database, and develop artificial intelligence analysis, to study disease progression pathways in preterm babies, causal modelling, surrogate outcome validation, and identification and mitigation of population-based biases.
Upcoming /Ongoing Projects within the Theme
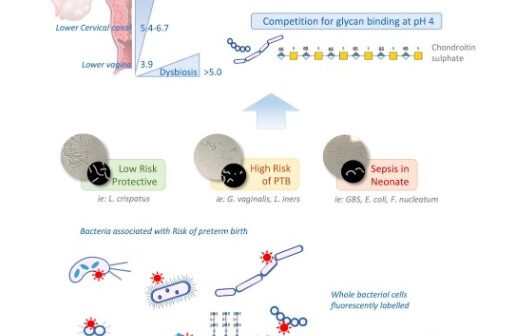
Miscarriage and spontaneous PTB research exploit our identification of potentially preventable adverse host-microbe interactions as drivers of cervical cancer, miscarriage and PTB. Using large cohorts of women at risk of both miscarriage and preterm birth, we will investigate interactions between reproductive tract microbiome, inflammation, decidual function, fetal membranes, cervix, and myometrium, endocrine, inter-pregnancy interval, nutritional and environmental influences. Deciphering glycan-mediation of microbiota-host interactions will lead to novel glycan-decoy therapeutics development. In collaboration with industry, we will conduct studies of vaginal and oral live biotherapeutics (probiotics), to improve reproductive tract microbial health. We will also explore anti-complement interventions to prevent miscarriage, PTB, preterm membrane rupture and improve neonatal outcomes.
Maternal-fetal cardiovascular intervention studies follow our findings that pre-pregnancy maternal cardiovascular function associates with pre-eclampsia/fetal growth restriction. In clinical intervention studies, we will optimise pre-pregnancy cardiovascular function in high-risk women through targeted exercise and oral organic nitrate vasodilators, and test the safety of S-nitrosoglutathione, which improves endothelial and platelet function in early-onset pre-eclampsia.
Optimising delivery timing in fetal growth restriction will involve 50 UK and European centres. Instrument development and completed proof-of-concept Super-Micro-Vascular Imaging and High-Intensity Focused Ultrasound HIFU in Twin-Twin Transfusion Syndrome will be translated into practice and extend to other fetoplacental and fetal vascular conditions such as Twin Reversed Arterial Perfusion syndrome and fetal sacrococcygeal and cervical teratoma.
Preterm neonate clinical studies will focus on cardiovascular stability and nutrition as key modifiable factors in neonatal outcomes and longer-term cardiometabolic health. We will examine splanchnic blood flow in transfusion-related necrotising enterocolitis; cardiovascular stability to predict acute collapse and brain injury; and enteral-parenteral nutrition on biomarkers of later cardiometabolic disease, vascular morphology; and body composition (using our gold-standard, neonatal whole-body MRI technique).
Neonatal data science studies will use our National Neonatal Research Database data-driven models targeting population stratification, disease progression pathways, causal modelling, surrogate outcome validation, and identification and mitigation of population-based biases. We will augment the value of the NNRD by incorporating physiological monitoring and imaging data to improve personalised risk predictions derived from artificial intelligence and machine learning analysis. We will develop NNRD-AI, a version curated and optimised for artificial intelligence and machine learning analysis and NNRD-Digital Twin, a “synthetic NNRD” which lacks specific patient identifiers and allows for confidentiality-free data exploration.
Statistical and technical developments will enable the National Neonatal Research Database to be used in the conduct of large clinical trials, enabling speedier data flows and assembly of clinical trial datasets from the NNRD, and shift the “one-trial-at-a-time” paradigm to testing multiple interventions simultaneously. This will enable efficient, large-scale, national, multicentre real-world data-enabled neonatal trials, assessing meaningful clinical outcomes with the power to identify sub-group and ethnicity effects. We will develop statistical models to avoid co-enrolment biases and examine different trial designs suitable for neonatal low-risk comparative-effectiveness and higher-risk interventional trials.
Long-term health studies of children born preterm and their mothers will integrate our densely phenotyped cohorts of women who have delivered pre-term, and of people who have been born to study factors underlying long-term health, multi-morbidity clustering, and relationships with ethnicity and underserved communities. We will create one of the world’s largest longitudinal, population-based, observational PTB cohorts, containing over half a million individuals linked to health (national statistics/Paediatric Intensive Care/Mental Health/Maternity) and non-health (air pollution/education) data. This will allow us to study globally relevant uncertainties not amenable to clinical trials, for example, the effects of the inter-pregnancy interval, alcohol or substance abuse, pollution, COVID-19 on stillbirth/PTB and infant health and educational outcomes, explore reduced PTB in disadvantaged socio-economic groups during COVID-19 lockdown and provide an international resource for long-term pregnancy-preterm studies which is a major pharmaceutical need.
Patient and Public Involvement, Engagement and Participation
Our theme will fund a full-time public-patient involvement and engagement lead to coordinate the establishment of a new Perinatal Evidence Collaborative. This will focus our several Patient and Public Involvement, Engagement and Participation groups into an integrated structure across all Theme activities with representation on our Theme management group. Public-patient involvement will involve not only the mothers of preterm children, but extended families, and adults who were themselves born preterm also.
Equality, Diversity and Inclusion
Our Themes’ commitment to equality, diversity and inclusion recognises that excellence comes with inclusive opportunities that bring together people with different experiences and backgrounds and that patient recruitment into studies is improved where the research delivery team has the same diversity as the populations that we study and serve. The theme is actively working to ensure equality, diversity and inclusion at every level, from research delivery staff to senior management.
Key Individuals
-
Professor Neena Modi
Theme Lead, Pregnancy & Prematurity -
Professor Phil Bennett
Theme Lead, Reproductive & Early Life Health -
Dr Beth Holder
Research Associate, Department of Medicine -
Dr Cheryl Battersby
Clinical Senior Lecturer in Neonatal Medicine -
Dr David MacIntyre
MRC-CDA Fellow & Lecturer in Reproductive Systems Medicine -
Dr Edward Mullins
Clinical Senior Lecturer in Obstetrics -
Dr James Webbe
Clinical Lecturer in Neonatal Population Health -
Dr Jayanta Banerjee
-
Dr Lynne Sykes
Clinical Reader in Obstetrics -
Dr Sabita Uthaya
Professor of Practice (Neonatal Medicine) -
Dr Vasso Terzidou
Clinical Reader in Obstetrics and Gynaecology -
Professor Chris Gale
Professor of Neonatal Medicine -
Professor Christoph Lees
Reader in Obstetrics & Fetal Medicine / Consultant in Obstetrics -
Professor Tom Bourne
Consultant Gynaecologist