Diagnostic ‘Transformative’ blood test could detect the cause of fever in children from molecular signatures
A simple blood test might be able to rapidly diagnose the cause of a child’s illness could be ‘transformative’, say researchers.
An international team of researchers, including a few supported by the NIHR Imperial BRC, has developed and validated a diagnostic approach capable of simultaneously detecting and distinguishing between 18 infectious or inflammatory diseases– including group B Streptococcus (GBS), respiratory syncytial virus (RSV) and tuberculosis – with the potential to provide a result in a fraction of the time of current diagnostic tests.
Using a single sample of blood, the test could enable clinicians to diagnose the cause of fever based on the distinctive pattern of genes being ‘switched on or off’ by the body in response to specific illnesses. A test, based on this approach would be capable of providing a result in under 60 minutes, whereas current tests for some conditions can take anything from several hours to weeks.
The researchers explain that while their study represents a proof-of-concept for the method, showing it works, a diagnostic test based on patients’ gene expression could drastically improve the diagnosis of childhood diseases, reduce delayed and missed diagnoses, and have a significant impact on healthcare, especially in developing regions.
The preliminary findings, published for the first time in the journal Cell Press Med, build on more than a decade of research to detect and diagnose illnesses based on patterns of gene expression. This foundational work led to the establishment of the DIAMONDS consortium in 2020, an international project funded by the EU Horizon2020 programme and led by Imperial College London to develop rapid diagnostic tests for febrile illnesses.
Professor Michael Levin, Chair in Paediatrics & International Child Health within the Department of Infectious Disease at Imperial College London, explains: “Despite huge strides forward in medical technology when a child is brought into hospital with a fever, our initial approach is to treat based on the doctors’ ‘impression’ of the likely causes of the child’s illness.”
“As clinicians, we need to make rapid decisions on treatment, often just based on the child’s symptoms, information from the parents, and our medical training and experience,” he adds, “but we may not know whether a fever is bacterial, viral, or something else until hours or days after a child has been admitted, when their test results come back. Such delays can stop patients from getting the right treatment early on, so there is a clear and urgent need to improve diagnostics. Using this new approach, once it’s translated to the near point of care devices, could be transformative for healthcare.”
Infectious and inflammatory diseases are the most common cause for children seeking medical care in hospitals, GP or community clinics. But with general symptoms such as fever, it can be difficult for clinical teams to reliably diagnose bacterial infections, which may be potentially life-threatening, from other causes, which may be less serious.
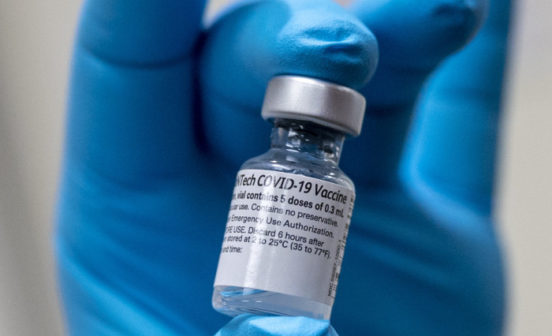
Often, patients may be given broad-spectrum antibiotics until a bacterial infection can be ruled out. However, this approach leads to the widespread overuse of antibiotics, ultimately contributing to antimicrobial resistance and increased drug-resistant infections.
Most diagnostic tests are focused on detecting pathogens – such as lateral flow tests (LFTs) for SARS-CoV-2, HIV or Influenza, or blood cultures to confirm the presence of bacteria or yeast. Although, LFTs can only provide a yes or no result for one of the possible causes of the illness, and blood cultures may take 72 hours or more to provide reliable results.
In the latest study, researchers explored an approach focused on detecting the pattern of a patient’s gene expression in blood that occurs in response to specific infections and inflammatory conditions. Using data from thousands of patients (including more than 1000 children with 18 infectious or inflammatory diseases) the team was first able to identify which key genes were switched ‘on’ or ‘off’ in response to a range of illnesses – providing a molecular signature of disease.
Machine learning was then applied to identify which patterns of gene expression corresponded to the specific disease areas and pathogens – focusing on a panel of 161 genes for 18 conditions. This panel was further validated in a cohort of 411 paediatric patients admitted to the hospital with sepsis or severe infections (representing 13 of the 18 diseases), where gene expression was captured from blood analysis and diagnoses were made using current gold standard clinical methods.
New diagnostic tests cannot be tested in a clinical setting until they are approved – as some misdiagnoses could have severe consequences, such as failing to identify a life-threatening bacterial infection. Instead, the team used a ‘cost sensitive’ measure, based on consensus from a panel of five clinical experts, to show where the test could be used to avoid misdiagnosis, and where this would have the greatest consequence.
Dr Myrsini Kaforou, Senior Lecturer within Imperial’s Department of Infectious Disease, said: “This body of work has enabled us to identify the molecular signature of a wide range of diseases based on 161 genes, out of thousands of genes in the human genome. By distinguishing between many diseases at the same time within the same test, we have developed a more comprehensive and accurate model that aligns with the way clinicians think about diagnosis.
“With this initial proof-of-concept study, we’ve been able to show that our multi-disease machine-learning diagnostic approach works. This kind of advance is only possible through interdisciplinary collaboration and large research consortia, which bring together expertise from infectious disease, molecular science, and bioinformatics.
“There is still much work to be done to progress this test to the clinic, but we are working towards it. A future diagnostic test based on this approach could help provide the right treatment, to the right patient, at the right time, while optimising antibiotic use, and reducing lengthy time to diagnosis for inflammatory diseases.”
The researchers stress that a functional test is not yet available for clinical practice and their RNA transcript panel would require further adaptation, testing and translation into a readily usable platform/device before it could be approved by regulators.
They highlight one potential advantage of their approach could help to rapidly diagnose respiratory illness, such as bacterial pneumonia or tuberculosis – while a pathogen-based blood test may not be effective (as the pathogen is in the lung, not the blood), a host-based test could still spot the tell-tale molecular signature it leaves in the patient’s blood, through the patient’s gene expression.
As part of the international, multi-partner DIAMONDS study, the next step is to trial the approach in thousands of patients in hospitals in Europe, Africa and Asia. This phase will assess the new approach against the current gold standard for clinical diagnosis, and how likely it is to change clinical decision making.
Dominic Habgood-Coote, a Research Associate within the Department of Infectious Disease at Imperial College London, said: “Using host transcriptional responses to disease is appealing for the diagnosis of fever in children, in whom traditional diagnostic approaches are particularly difficult. We have shown our approach is useful in answering narrowly defined clinical questions, but there is a clear benefit to expanding it to include a wider range of diseases and more detailed classification.”
Professor Levin, added: “Fundamentally, I’m a clinician, and the reason we do research is that we want something better for the patients. I think the excitement around this platform is the clinical implication. If we can move it into clinical use, it really could transform health services.”