Treatment Flexible hepatitis C treatments could pave the way for elimination
In the first head-to-head comparison of recommended hepatitis C treatments, researchers from Imperial College London have provided key evidence to support global efforts to eliminate the disease. Their findings have also helped uncover new ways to treat hepatitis C that could make it easier for more people to access and complete curative treatment.
The findings, published in The Lancet, confirm that current World Health Organisation (WHO)-recommended drug combinations for hepatitis C are highly effective, while also showing that alternative strategies, like shorter courses or taking treatment breaks, can still lead to successful outcomes.
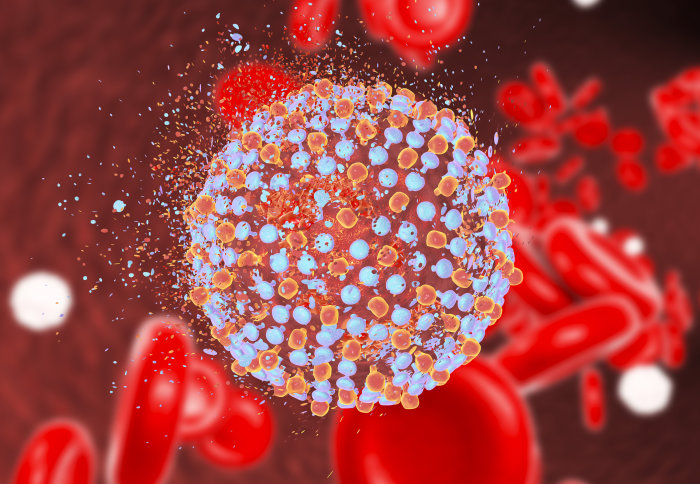
Hepatitis C is a viral infection that affects the liver and can lead to serious complications (including liver cancer and cirrhosis) if untreated. It is spread through blood-to-blood contact and disproportionately affects marginalised communities around the world. In 2016, WHO set a goal to eliminate hepatitis C as a public health threat by 2030—but challenges remain.
The VIETNARMS trial—funded by the Wellcome Trust and led by investigators from Imperial College London in collaboration with, MRC Clinical Trials Unit and Oxford University Clinical Research Unit in Vietnam—enrolled over 600 adults with chronic hepatitis C. The trial was conducted at two major Vietnamese hospitals, the Hospital for Tropical Diseases in Ho Chi Minh City and the National Hospital for Tropical Diseases in Hanoi. It focused on two key questions:
- Which of the WHO-recommended treatments works best in people with mild-to-moderate disease?
- Can we make treatment easier to access and complete without reducing the chances of cure?
Comparing two trusted treatments
Participants were randomly assigned to take one of the two WHO-recommended drug combinations: Sofosbuvir–daclatasvir (SOF/DCV) and sofosbuvir–velpatasvir (SOF/VEL).
The trial showed that both treatments worked extremely well, even among people with genotype 6, a rarer strain of hepatitis C that’s common in Vietnam. Despite previous concerns, both drug combinations were equally effective across all hepatitis C types.
Although previously considered less effective, SOF/DCV slightly outperformed SOF/VEL, with 97.4% of patients cured compared to 95.1%, and a 93% chance that it was the more effective of the two. This new head-to-head evidence could help countries make better-informed decisions about which treatment to prioritise, particularly where drug prices vary significantly.
Flexible treatment options
To support patients who may struggle to complete the standard 12-week course, due to cost, treatment burden, or challenges such as substance dependency or mental health conditions, an innovative trial design also tested four alternative treatment strategies using both drug combinations:
- Standard-of-care: Daily DAA tablets for 12 weeks (the current global standard)
- Induction-maintenance: Daily tablets for two weeks, then just five days a week (weekends off) for 10 more weeks injectable pegylated interferon (PEG-IFN): Four weeks of tablets, plus weekly injections of a drug called PEG-IFN
- Response-guided: After one week of daily DAA tablets, participants’ viral response to treatment is measured. Based on this, participants either continued treatment for four, eight, or the full 12 weeks.
Compared to the standard-of-care, the alternative strategies used in the trial involved fewer tablets and were easier for people to stick to. All of these strategies were non-inferior to standard-of-care, meaning they were not worse than standard-of-care by more than a pre-specified amount (10%).
The most effective alternative was the “induction maintenance” approach—this cured 99.3% of people, slightly more than the standard 12-week treatment, which cured 98.7%
The other two strategies also worked well. The PEG-IFN option, which combined tablets with weekly injections, cured 94.1% of participants. The response-guided approach, which adjusted treatment length based on how people responded in the first week, cured 92.9%.
However, people in the response-guided group who stopped treatment after just four weeks didn’t do as well, even if they showed a strong early response. This confirms earlier findings that four weeks of tablets alone isn’t enough for most people. Interestingly, the PEG-IFN group, who also had only four weeks of tablets, still had high cure rates, showing the added injections helped make the treatment more effective.
Global impact
By showing that shorter or more flexible treatment plans can still cure hepatitis C, the VIETNARMS trial opens the door to new approaches that could better meet people’s needs, particularly those with limited access to care, or who face challenges like mental health issues or substance use.
The results also provide clear evidence for governments, doctors and global health organisations to consider a broader range of options in national treatment programmes—while also potentially lowering the cost of care.
Professor Graham Cooke, senior author, Deputy Dean of the Faculty of Medicine at Imperial and NIHR Imperial BRC Infection and AMR Theme Co-lead, said: “We expect this new evidence will help countries, clinicians and patients in the decisions they need to make if we are to achieve the ambitious WHO elimination targets for hepatitis C. By showing that a range of flexible and effective treatment options are possible, we hope our findings can support more inclusive, accessible and cost-effective care—especially in communities where treatment completion has been a challenge.”





