DiagnosticPrevention Blood pressure variability- a major predictor of heart attack and stroke risk
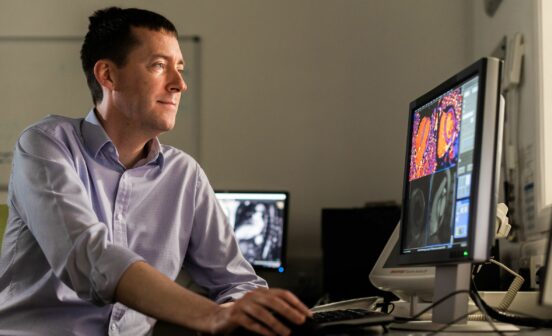
Changes in blood pressure over time could be used to identify patients at greatest risk of heart attack and stroke. These are the findings of a new analysis from the ASCOT study, led by researchers from Imperial College London, including Professor Peter Sever who is supported by the NIHR Imperial BRC, and published in the European Heart Journal.
It reveals that patients with blood pressure that varies significantly from one doctor’s visit to the next may be at greater risk of cardiovascular events compared to those with high blood pressure but low variability which is kept under control with medication.
In a group of more than 8,000 UK patients with high blood pressure who were followed up for more than 20 years, researchers found that variation in systolic pressure (the larger of the two numbers used to measure blood pressure) over time was a strong predictor of stroke, heart attack and atrial fibrillation. High variability of blood pressure was also a strong predictor of risk at all levels of average blood pressure from low to high.
The team behind the study is calling for medical guidelines to be changed to focus not only on the measurement of a patient’s blood pressure but how it varies from visit to visit, to intervene earlier and reduce risk.
The researchers also highlight that data from the trial show that one blood pressure medication, a drug called amlodipine, was effective in lowering blood pressure variability and could help to reduce risk.
Professor Sever, senior author of the study from the National Heart & Lung Institute at Imperial College London, said: “We’ve long known that high blood pressure increases the risk of heart attacks and stroke, but our latest findings highlight the importance of tracking variability in blood pressure over time as well.
“While a degree of this was known to doctors, without clinical trials it has been difficult to quantify the risk of blood pressure variability over the long term, or the impact of interventions such as calcium blockers to reduce patients’ risk.”
Hypertension
High blood pressure, or hypertension, is a leading cause of death and disability worldwide – contributing to millions of strokes and heart attacks. An estimated 1.28 billion people have hypertension around the world, affecting 1 in 3 adults. Using new definitions for hypertension (blood pressure of more than 130/80 mmHg) this rate increases to almost 50% of all adults. The condition can be well-controlled with medications, including ACE-inhibitors, calcium channel blockers, diuretics and beta-blockers.
It is well-established that blood pressure can vary over the course of the day. For example, ambulatory blood pressure monitoring requires a patient to wear a device at home to take their average blood pressure levels over a 24-hour period, which can be used by their doctor to help with treatment decisions. But the impact of blood pressure variability over the longer term, from one doctor’s visit to the next, has been less clear.
Professor Peter Sever, who leads the ASCOT Legacy trial, added: “We urgently need to explore new practical ways to assess blood pressure variability and are currently studying the possibilities of incorporating data from home blood pressure monitoring into clinical decision-making.
“The low cost and wide availability of digital blood pressure monitors and health apps means people can readily track their blood pressure over time and this could provide invaluable data for doctors to make the best treatment decisions – though we’d urge patients not to be overly concerned, as we would expect a degree of variation in their readings over time.
“Crucially, we need international guidelines for clinicians to be updated to reflect these latest findings and to include blood pressure variability as a major risk factor for heart attack and stroke.”
In the latest study, researchers used data from the ASCOT study, which involved more than 1 million measurements of blood pressure in almost 20,000 participants observed for over 5 years and up to 21 years of follow-up data. From the original ASCOT study, 8,580 participants from England, Wales and Scotland were included in the ASCOT Legacy Study and followed up until 2019, during which period 717 of them died. The majority of patients were male (81%) and the average age was 64 years old at the start of the study, and half were taking a calcium channel blocker called amlodipine to manage their hypertension.
Analysing blood pressure
In the analysis, the team split the group into thirds, based on their average systolic blood pressure and their blood pressure variability. They found that among patients with an average systolic blood pressure of less than 140 mmHg, the group with the highest variability was at a 16% greater risk for heart attacks, strokes and other cardiovascular events compared with the group with the lowest variability.
It also showed that more than half (53%) of all cardiovascular events occurred in patients whose blood pressure was well-controlled with medication and who would not have been considered for additional treatment under the guidelines in place at the time of the trial (i.e. with medication they achieved a systolic blood pressure of <140 mmHg). Some European guidelines now recommend a lower target for systolic pressure of 130-135 mmHg, but even applying these values those with high blood pressure variability still have a considerable excess of heart attacks and strokes.
The findings indicate that a systolic blood pressure variability of 13 mmHg or more over the course of five years may be associated with a significantly increased risk of cardiovascular events.
In the original ASCOT trial, researchers showed that amlodipine-based treatment was better than a beta-blocker-based treatment strategy for preventing heart attacks and strokes and that this benefit was best explained by the effect of amlodipine on reducing blood pressure variability. Other studies have now confirmed amlodipine’s beneficial effect on blood pressure variability. Of the other classes of blood pressure-lowering drugs, only thiazide-like diuretics have some beneficial effect on blood pressure variability.
Professor Sever added: “We still don’t know what the optimum method for capturing blood pressure variability over time looks like – whether this may incorporate office and home measurements to best inform a patient’s health record in the long term – and more research is needed.
“Whilst new trials are necessary to confirm the benefits of drugs which lower blood pressure variability, in the meantime our best evidence is that in patients with high variability, a treatment regimen that includes a long-acting calcium channel blocker such as amlodipine is the sensible option.”