Diagnostic Detailed map of the human heart provides insights into cardiac disease

In a new study, researchers, including some funded by NIHR Imperial BRC, have produced the most detailed and comprehensive human Heart Cell Atlas to date, including the specialised tissue of the cardiac conduction system which is where the human heartbeat originates.
The multi-centre team is led by the Wellcome Sanger Institute and the National Heart and Lung Institute (NHLI) at Imperial College London and has also presented a new drug-repurposing computational tool called Drug2cell, which can provide insights into the effects of drugs on heart rate. The study was partially supported by the Imperial College Healthcare Tissue Bank, a facility funded by the NIHR Imperial BRC.
This study is part of the international Human Cell Atlas (HCA) initiative, which is mapping every cell type in the human body, to transform our understanding of health and disease, and will form the foundation for a fully integrated HCA Human Heart Cell Atlas.
Charting eight regions of the human heart, the work describes 75 different cell states including the cells of the cardiac conduction system (the group of cells responsible for the heartbeat) not understood at such a detailed level in humans before. The human cardiac conduction system, the heart’s ‘wiring’, sends electrical impulses from the top to the bottom of the heart and coordinates the heartbeat.
By using spatial transcriptomics, which gives a ‘map’ of where cells sit within a tissue, researchers were also able to understand how these cells communicate with each other for the first time. This map acts as a molecular guidebook, showing what healthy cells look like, and providing a crucial reference to understand what goes wrong in disease. The findings will help us understand diseases such as those affecting the heart rhythm.
The assembly of a Human Heart Cell Atlas is key given that cardiovascular diseases are the leading cause of death globally. Around 20,000 electronic pacemakers are implanted each year in the UK for these disorders. These can be ineffective and are prone to complications and side-effects. Understanding the biology of the cells of the conduction system and how they differ from muscle cells paves the way to therapies to boost cardiac health and develop targeted treatments for arrhythmias.
Drug insights
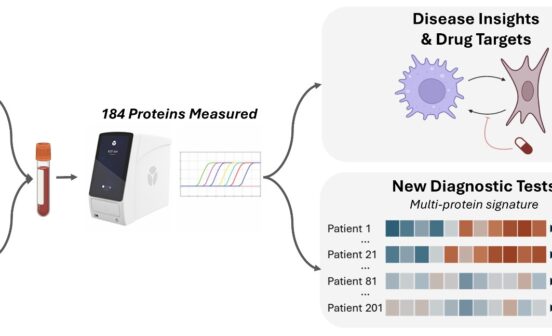
The team also presents a new computational tool called Drug2cell. The tool can predict drug targets as well as drug side effects. It leverages single-cell profiles and the 19 million drug-target interactions in the EMBL-EBI ChEMBL database.
Dr Michela Noseda, senior Lecturer in Cardiac Molecular Pathology at the NHLI, Imperial and a lead author, said: “We often don’t fully know what impact a new treatment will have on the heart and its electrical impulses – this can mean a drug is withdrawn or fails to make it to the market. Our team developed the Drug2cell platform to improve how we evaluate new treatments and how they can affect our hearts, and potentially other tissues too. This could provide us with an invaluable tool to identify new drugs which target specific cells and help predict any potential side-effects early on in drug development”.
Unexpectedly, this tool identified that pacemaker cells express the target of certain medications, such as GLP1 drugs, which are used for diabetes and weight loss and are known to increase the heart rate as a side-effect, the mechanism of which was unclear. This study suggests that the increase in heart rate might be partly due to a direct action of these drugs on pacemaker cells, a finding the team also showed in an experimental stem cell model of pacemaker cells.
Dr James Cranley, a cardiologist specialising in heart rhythm disorders and PhD student at the Wellcome Sanger Institute, said: “The cardiac conduction system is critical for the regular and coordinated beating of our hearts, yet the cells which make it up are poorly understood. This study sheds new light by defining the profiles of these cells and the multicellular niches they inhabit. This deeper understanding opens the door to better, targeted anti-arrhythmic therapies in the future.”
Surprise surprise
The study unearthed an unexpected discovery, a close relationship between conduction system cells and glial cells. Glial cells are part of the nervous system and are traditionally found in the brain. They have been explored very little in the heart. This research suggests that glial cells are in physical contact with conduction system cells and may play an important supporting role – communicating with the pacemaker cells, guiding nerve endings to them, and supporting their release of glutamate, a neurotransmitter.
Another key finding of the study is an immune structure on the heart’s outer surface. This contains plasma cells, which release antibodies into the space around the heart to prevent infection from the nearby lungs. The researchers also identified a cellular niche enriching for a hormone that could be interpreted as an early warning sign of heart failure.
Professor Metin Avkiran, Associate Medical Director at the British Heart Foundation, which part-funded the research with the German Centre for Cardiovascular Research (DZHK), said “International collaboration is key to scientific progress. This impactful study and other discoveries from the broader Human Cell Atlas initiative are excellent examples of what can be achieved when the international research community works together across borders. Our combined efforts can ultimately produce better outcomes for patients worldwide”.