Diagnostic Research advancement could liberate brain cancer patients from risky surgery
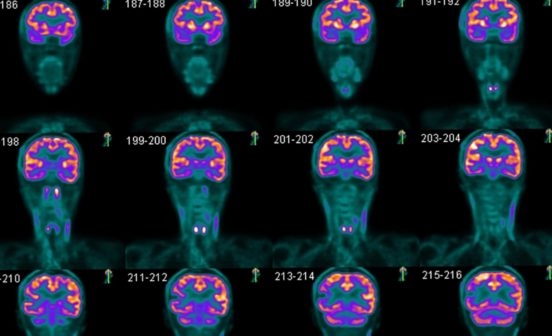
A simple blood test could help diagnose patients with the deadliest form of brain cancer, sparing them from undergoing invasive and dangerous surgery, according to the findings of a clinical validation study published in the International Journal of Cancer. The study was led by Imperial researchers and clinicians, including Dr Nelofer Syed from the NIHR Imperial BRC Brain Sciences Theme.
In a world-first, the new technique has been proven for glial tumours including glioblastoma (GBM), the most commonly diagnosed type of high-grade brain tumour in adults.
The findings of the study involving brain tumour patients, which took place at the Brain Tumour Research Centre of Excellence run by Imperial College London and Imperial College Healthcare NHS Trust, could make a huge difference to patients with suspected high-grade gliomas, including GBM, astrocytomas, and oligodendrogliomas, leading to earlier diagnosis of their tumour type, speedier treatment, and potentially increasing survival rates. It could also eliminate the need for surgical biopsies which carry significant risk, particularly for those with underlying health conditions.
Crucially, in addition to speeding up diagnoses in patients who cannot have biopsies – which is vital for fast-growing, highly aggressive cases – this new technology is inexpensive and simple to implement within clinics, meaning it could easily be adopted to improve care.
The work, funded by Datar Cancer Genetics, has already attracted the attention of the body responsible for advancing public health in the US, the Food and Drug Administration (FDA). Hopes are now of a larger study here in the UK which, if successful, could mean patients with suspected high-grade tumours benefit from this breakthrough in as little as two years.
Dr Nelofer Syed, who leads the Brain Tumour Research Centre of Excellence at Imperial, said: “A non-invasive, inexpensive method for the early detection of brain tumours is critical for improvements in patient care.
“There is still some way to go, but this solution could help people where a brain biopsy or surgical resection of the tumour is not possible due to the location of the tumour or other constraints.
“Through this technology, a diagnosis of inaccessible tumours can become possible through a risk-free and patient-friendly blood test. We believe this would be a world-first as there are currently no non-invasive or non-radiological tests for these types of tumours.”
Kevin O’Neill, consultant neurosurgeon at Imperial College Healthcare and honorary clinical senior lecturer at Imperial College London, who leads the Brain Tumour Research Centre of Excellence alongside Dr Syed said: “This test is not just an indicator of disease, it is a truly diagnostic liquid biopsy. It detects intact circulating tumour cells from the blood, which can be analysed to the same cellular detail as an actual tissue sample. It’s a real breakthrough for treatment of brain cancers that rarely spread around the body.
“This could help speed up diagnosis, enabling surgeons to apply tailored treatments based on that biopsy to increase patients’ chances of survival. I’m very grateful to everyone who has contributed to this study, especially the patients involved.”
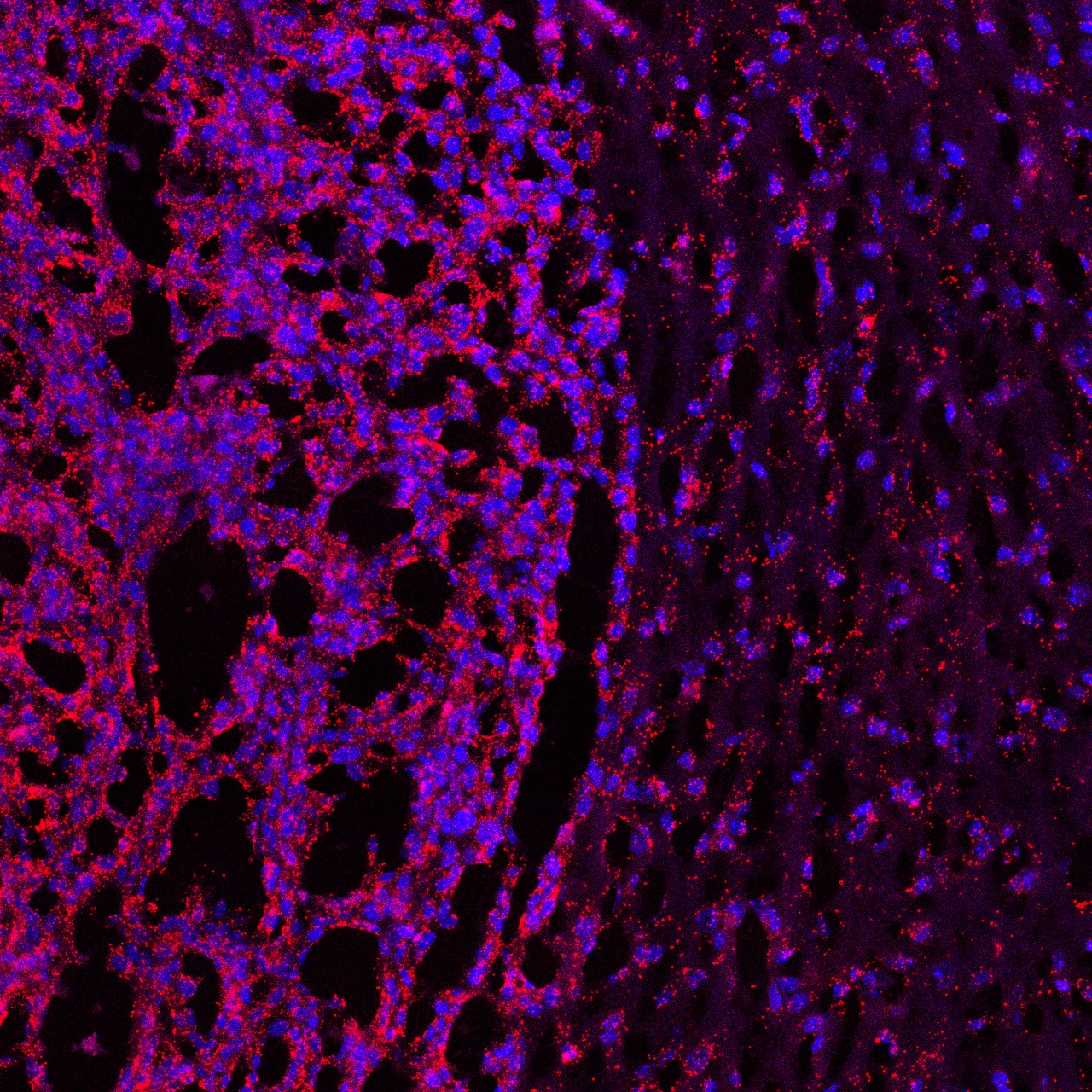
The TriNetra-Glio blood test works by isolating tumour cells that have broken free from the tumour circulating in the blood. The isolated cells are then stained and can be identified under a microscope.
GBM patient Steve Ackroyd, a TV editor from Palmers Green, North London, was initially misdiagnosed with and treated for epilepsy, with his brain tumour diagnosis coming three months later, in August 2022. The 47-year-old, who has a 12-year-old daughter, had a biopsy followed by radiotherapy and chemotherapy and is currently undergoing immunotherapy treatment in Germany which could cost as much as £300,000, financed through a crowdfunding page set up by his wife Francesca.
She said: “In Steve’s case he went through a surgical biopsy to determine his tumour type, and we also found out that its diffuse nature meant it was inoperable. We waited seven weeks for the results only to find out that the tissue was later deemed to be a ‘poor sample.’ Unfortunately, all the delays cost us precious time when he could have been on treatment.”
The findings are particularly significant as less than 1% of patients with GBM live for more than 10 years and, for many, the prognosis is as little as 12 months.
Dan Knowles, CEO of Brain Tumour Research, said: “This groundbreaking research could lead to earlier diagnosis and improved outcomes for brain tumour patients. The research undertaken in UK universities is world-class and something we should all be proud of, but we need so much more. There is an urgent need for novel approaches, particularly in the treatment of GBM, which is fatal in most cases. Brain tumours kill more people in the UK under the age of 40 than any other cancer and we have to find a cure for this devastating disease.
“It is scandalous to think that there have been no improvements to treatment options for this type of tumour in two decades and the standard of care for GBM patients – surgical resection followed by radiotherapy and chemotherapy – remains unchanged.
“This is why we are campaigning for the Government and larger charities to invest more and we will keep up the pressure until patients and their families get the help they so desperately need.”
Brain tumours kill more children and adults under the age of 40 than any other cancer yet just 1% of the national spend on cancer research has been allocated to this devastating disease since records began in 2002
Brain Tumour Research funds sustainable research at dedicated centres in the UK. It also campaigns for the Government and the larger cancer charities to invest more in research into brain tumours to speed up new treatments for patients and, ultimately, to find a cure. The charity is calling for a national annual spend of £35 million to improve survival rates and patient outcomes in line with other cancers such as breast cancer and leukaemia.