InnovationTherapeutic ‘Off-the-shelf’ immunotherapy for cancer
Pre-clinical evaluation of a novel immunotherapy treatment developed by Imperial researchers demonstrated potent anti-cancer properties
Immunotherapy is a personalised treatment where patient’s own immune cells are programmed to attack cancer cells. Immune cells called T cells are extracted from patient’s blood and are genetically manipulated to insert CAR (chimeric antigen receptor), which recognises cancer cells. These cells are grown in a lab and are subsequently injected into the patient as a therapy called CAR-T. However currently CAR-T therapy is very expensive (~£300,000 per patient), as this meticulous cell engineering procedure must be tailored to every patient.
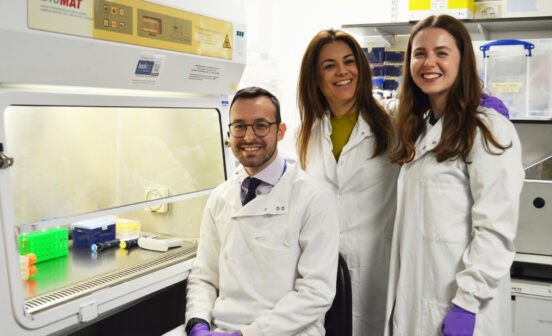
NIHR Imperial BRC Cancer Theme researchers used a different type of immune cell, called iNKT (invariant natural killer T-cell), to engineer a unique version of this type of therapy, called CAR19-iNKT. Dr Antonia Rotolo, first study author and a BRC-funded clinical research fellow, explained: “The current methods of producing CAR-T cells use the patient’s own T cells. However, iNKT-cells can be sourced from healthy individuals, and unlike T cells don’t need to be matched to the patient. This means CAR19-iNKT cell treatment can be used off-the-shelf”.
In a study published in Cancer Cell, authors used lymphoma pre-clinical models to assess anti-cancer efficacy of this novel therapy. They found that CAR19-iNKT eliminated cancer in 60% of subjects using a single dose, with 90% surviving long-term, thereby outperforming conventional CAR-T approach. Interestingly, CAR19-iNKT cells were able to infiltrate brain tissue, and tackle large tumours, which opens the possibility of utilising this approach for targeting brain tumours as well as brain lymphoma.
This work is led by Professor Anastasios Karadimitris, a BRC investigator based at Imperial’s Centre for Haematology, who commented on the potential of this therapy: “Cancer researchers and doctors are very excited about this therapy – it means that instead of talking to patients about a hospice, we can offer them a treatment that has a good chance of working.”
The study was supported in early stage by Imperial’s Confidence-in-Concept scheme and was developed and matured with funding from charity Bloodwise. Imperial Innovations, the College’s technology commercialisation partner, has patented the underlying cell engineering technology and is working with Professor Karadimitris on commercial applications.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.