Prevention Reversal of CPI-colitis by targeting IFNγ-producing immune cells provides hope for improved outcomes for cancer patients
A new study from Imperial researchers, including the NIHR Imperial BRC Digestive Diseases Theme Leads Professor Julian Marchesi and Dr Nick Powell, suggests that targeting the immune cells producing IFNγ, or the regulatory circuits that control these cells, may hold the key to reversing Immune checkpoint inhibitor (CPI)-colitis.
CPIs are relatively new cancer drugs that work by ‘activating’ the immune system to target cancer cells. However, they inadvertently trigger immune cells in other organs, causing severe immune-mediated damage. The intestines are one of the most common organs affected by these off-target adverse events. CPI-colitis causes disabling symptoms and can be life-threatening.
CPI impact on the intestinal immune system
To understand how CPIs affect the intestinal immune system, scientists from the Department of Metabolism, Digestion and Reproduction developed new preclinical models of disease based on the most commonly used immunotherapies, anti-CTLA4 and anti-PD-1, together with alterations in the makeup of the microbes living in their intestines.
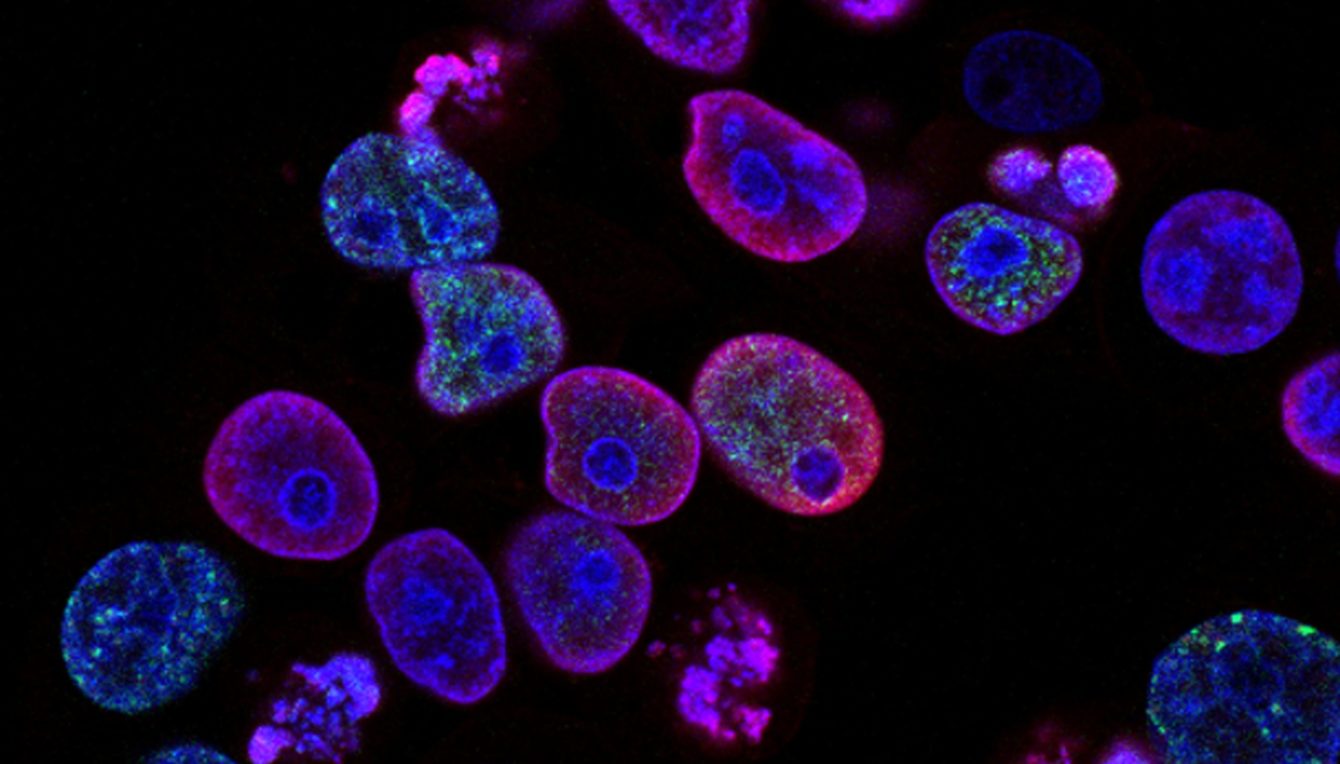
By scrutinising the colonic immune system following induction of CPI-induced colitis, they found that lymphocytes producing interferon-γ (IFNγ), cytotoxic molecules, and other inflammation-related substances, were key causative cells responsible for driving disease. Critically, they discovered that blocking the IL23/IFNγ pathway could effectively treat colitis.
Speaking about the findings and their potential impact, study lead, Professor Nick Powell said: “Although immunotherapy is a game-changing treatment for many cancer patients, it has an important Achilles heel. I now see many patients in my clinic with severe intestinal symptoms and serious complications of immunotherapy-induced colitis. Treatment options for CPI colitis are limited.
“Our work has identified a population of cells likely to be causing colitis. We were able to suppress these harmful cells by blocking a key chemical called interleukin-23. By treating mice with CPI-colitis with an antibody that neutralised interleukin-23 we could starve these harmful cells of one of their activating signals and limit the severity of colitis. This is an important discovery because drugs that block interleukin-23 are now emerging into clinical practice to treat other diseases, such as Crohn’s disease and ulcerative colitis. Hence, our findings could herald a new treatment paradigm for CPI-colitis”.





